August 20 is World Mosquito Day, a day to remind people that mosquitoes are one of the main vectors of disease transmission.
On August 20, 1897, the British microbiologist and physician Ronald Ross (1857-1932) discovered in his laboratory that mosquitoes were the vectors of malaria, and he pointed out an effective way to avoid malaria: stay away from mosquito bites. Since then, World Mosquito Day has been celebrated on August 20 each year to raise public awareness of malaria and other mosquito-borne diseases.
What are the main infectious diseases caused by mosquito bites?
01 Malaria
Malaria is an insect-borne infection caused by the infection of malaria parasites through the bite of Anopheles mosquitoes or through the transfusion of the blood of a malaria carrier. The disease is mainly manifested as periodic regular attacks, the whole body chills, fever, hyperhidrosis, long-term multiple attacks, can cause anemia and spleen enlargement.
The global prevalence of malaria remains high, with about 40 per cent of the world’s population living in malaria-endemic areas. Malaria remains the most serious disease on the African continent, with some 500 million people living in malaria-endemic areas, 90 per cent of them on the continent, and more than 2 million people dying from the disease each year. Southeast and central Asia are also areas where malaria is endemic. Malaria is still endemic in Central and South America.
Introduction to Malaria rapid test:
Malaria Pf Antigen rapid test is a side-flow chromatography immunoassay used to qualitatively detect Plasmodium falciparum (Pf) specific protein, histidine rich protein II (pHRP-II), in human blood samples. The device is intended to be used as a screening test and as an adjunct to diagnosing plasmodium infection. Any reactive sample that is rapidly tested using Malaria Pf Antigen must be confirmed using alternative testing methods and clinical findings.
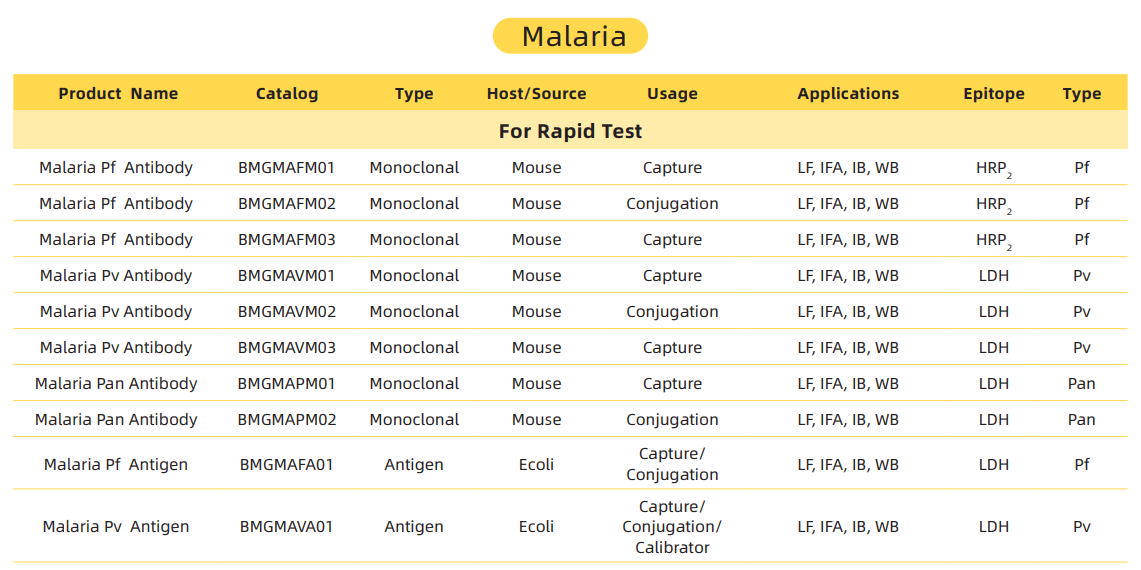
Malaria rapid test products recommended:
02 Filariasis
Filariasis is a parasitic disease caused by filariasis parasitizing human lymphatic tissue, subcutaneous tissue or serous cavity. Among them, Malay filariasis, Bancroft filariasis and lymphatic filariasis are closely related to mosquitoes. The disease is transmitted by blood-sucking insects. The signs and symptoms of filariasis vary according to the location of filariasis. The early stage is mainly lymphangitis and lymphadenitis, and the late stage is a series of symptoms and signs caused by lymphatic obstruction. Rapid test is mainly based on the detection of microfilaria in blood or skin tissue. Serological examination: detection of filarial antibodies and antigens in serum.
Introduction to filarial rapid test:
The filarial Rapid diagnostic test is a test based on the principle of immunochromatography that can diagnose filarial infection within 10 minutes by detecting specific antibodies or antigens in a blood sample. Compared with traditional microfilaria microscopy, rapid diagnostic detection of filaria has the following advantages:
1. It is not limited by blood collection time, and can be tested at any time, without the need to collect blood samples at night.
2. Do not need complex equipment and professional personnel, simply drop blood into the test card, and observe whether there is a color band to judge the result.
3. Without interference from other parasitic infections, it can accurately distinguish different types of filarial infections, and judge the degree and stage of infection.
4. It can be used for mass screening and monitoring of prevalence, as well as evaluating the effect of preventive chemotherapy.
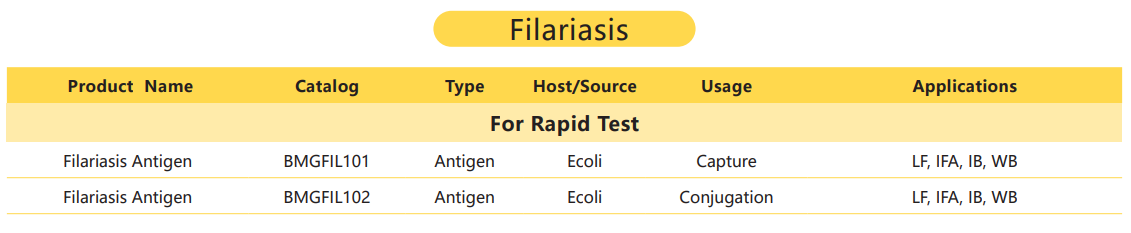
Filariasis rapid test products recommended:
03 Dengue
Dengue fever is an acute insect-borne infectious disease caused by Dengue virus and transmitted by the bite of the Aedes mosquito. The infectious disease is mainly prevalent in tropical and subtropical regions, especially in Southeast Asia, the Western Pacific region, the Americas, the eastern Mediterranean and Africa.
The main symptoms of dengue fever are sudden high fever, “triple pain” (headache, eye pain, generalized muscle and bone pain), “triple red syndrome” (flushing of the face, neck and chest), and rash (congestive rash or spot bleeding rash on the extremities and trunk or head and face). “The dengue virus and the virus that causes COVID-19 can cause similar symptoms early on,” according to the U.S. Centers for Disease Control (CDC) website.
Dengue fever occurs in summer and autumn, and is generally prevalent from May to November in the Northern Hemisphere every year, which is the Aedes mosquito breeding season. However, in recent years, global warming has put many tropical and subtropical countries at risk of early and expanded transmission of dengue virus.
Introduction to Dengue rapid test:
Dengue IgG/IgM Rapid assay is a side-flow chromatography immunoassay used to qualitatively detect dengue virus IgG/IgM antibodies in human serum, plasma, or whole blood.
Test material
1. Testing procedures and interpretation of test results must be closely followed when testing individual subjects for the presence of antibodies to dengue virus in serum, plasma or whole blood. Failure to follow this process may produce inaccurate results.
2. Rapid detection of dengue IgG/IgM combination is limited to qualitative detection of dengue virus antibodies in human serum, plasma or whole blood. There was no linear correlation between the strength of the test band and the antibody titer in the specimen.
3. The rapid dengue IgG/IgM combination test cannot be used to distinguish between primary and secondary infections. The test does not provide information on dengue serotype.
4. Serologic cross-reactivity with other flaviviruses (e.g., Japanese encephalitis, West Nile, yellow fever, etc.) is common, so patients infected with these viruses may show some degree of reactivity through this test.
5. Negative or non-reactive results in individual subjects indicate no detectable dengue virus antibodies. However, negative or non-reactive test results do not rule out the possibility of exposure or infection with dengue virus.
6. If the number of dengue virus antibodies present in the specimen is below the detection line, or if no detectable antibodies are present at the stage of disease at which the specimen was collected, a negative or non-reactive result may occur. Therefore, if clinical manifestations strongly suggest an infection or outbreak, follow-up tests or alternative tests, such as antigen tests or PCR test methods, are recommended.
7. If symptoms persist, despite negative or non-responsive results from the combined IgG/IgM rapid test for dengue, it is recommended that the patient be resambused a few days later or tested with alternative testing equipment.
8. Some specimens containing unusually high titers of heterophile antibodies or rheumatoid factors may affect the expected results.
9. The results obtained in this trial can only be interpreted in conjunction with other diagnostic procedures and clinical findings.
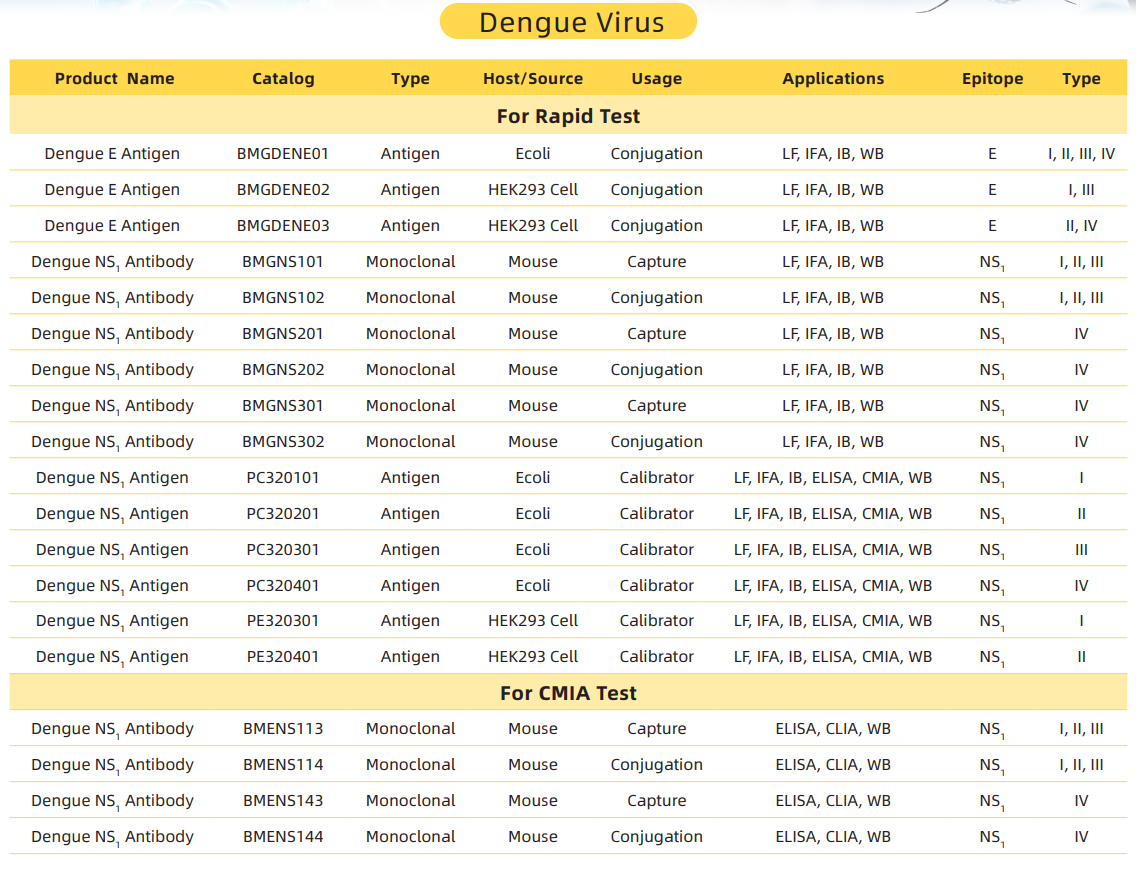
Dengue rapid test products recommended:
Using boat-bio rapid diagnostic tests can improve diagnostic efficiency and accuracy, which is conducive to timely detection and treatment of infected people, so as to control and eliminate these harmful parasitic diseases.
boat-bio’s rapid test products enable rapid and accurate detection of the disease.
Post time: Aug-15-2023